A new analysis of the Affordable Care Actfs health insurance marketplace
costs finds that, nationwide, marketplace premiums did not increase at all from
2014 to 2015, though there were substantial average premium increases in some
states and declines in others. This weighted analysis is the most comprehensive
to date as it examines:
The average premiums for the second lowest-cost silver plan—or benchmark plan
for calculating the federal subsidy in a given state—were also unchanged. And
the average deductible for a marketplace plan increased by just 1 percent year
to year.
The premiums presented are for a 40-year-old nonsmoker. Results are weighted
to reflect the population distribution across rating regions. The data for
single and family premiums are available in an interactive
map.
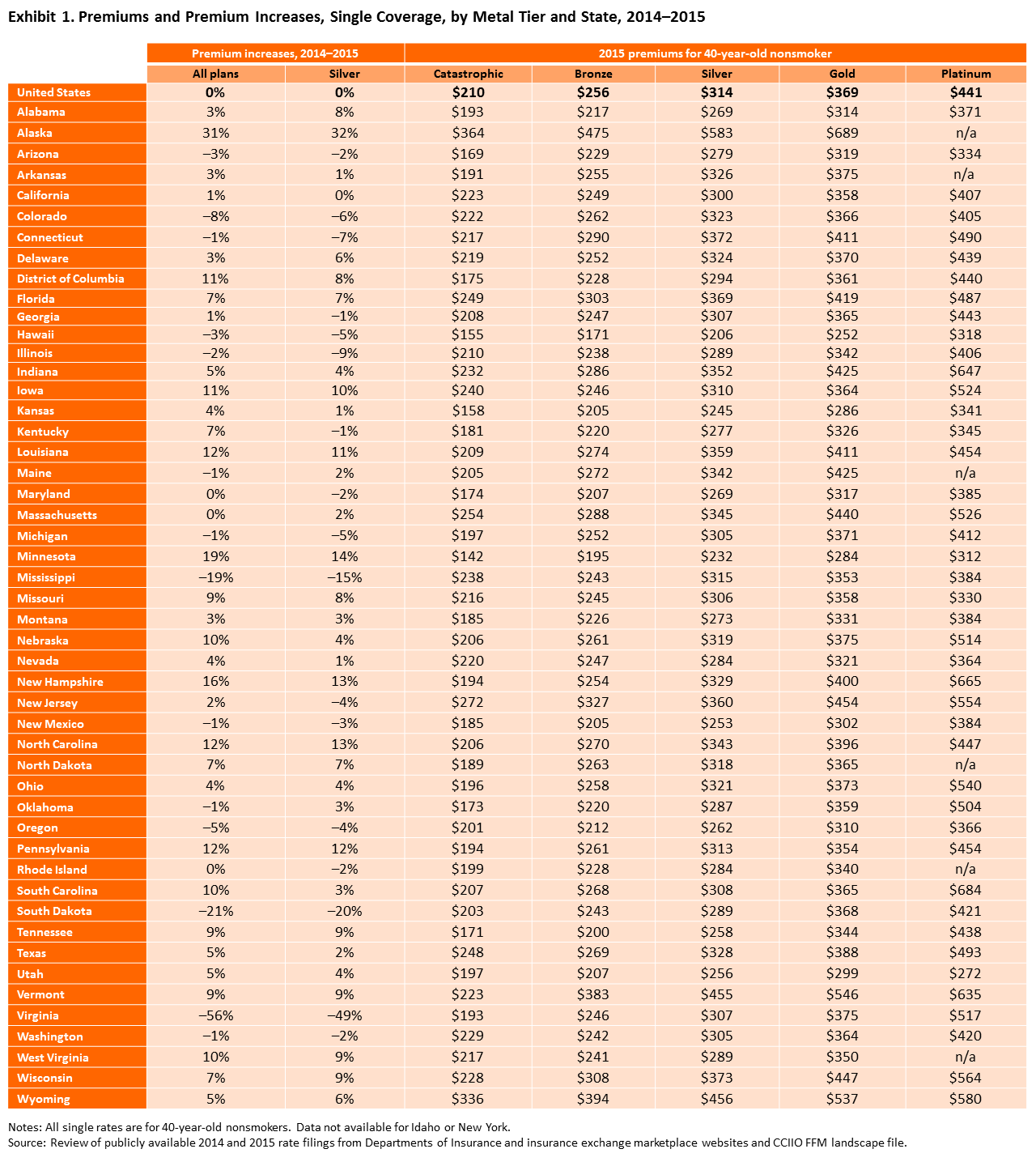
While average premiums nationwide did not change from 2014 to 2015, there
were wide differences across states (Exhibit 1). There were double-digit
increases in 10 states plus the District of Columbia (Alaska, the District of
Columbia, Iowa, Louisiana, Minnesota, Nebraska, New Hampshire, North Carolina,
Pennsylvania, South Carolina, and West Virginia). Average premiums declined in
14 states (Arizona, Colorado, Connecticut, Hawaii, Illinois, Maine, Michigan,
Mississippi, New Mexico, Oklahoma, Oregon, South Dakota, Virginia, and
Washington).
In certain states, those double-digit increases and decreases can be tied to
a single insurer decision. In Minnesota, the state with the lowest premiums
nationally in 2014, PreferredOne—the carrier with the lowest statewide premiums
and largest market share—exited the market, driving up the average cost of a
marketplace plan. In Virginia, Optima Health, a carrier charging $2,000 a month
for a silver plan, a figure nearly seven times the cost of the
average silver plan, dropped this expensive plan, thereby sharply decreasing the
average cost for plans in Virginia.
In other states, entry by multiple carriers enhanced price competition, which
made shopping around a good approach for consumers in the second enrollment
period. In Georgia, Cigna, Coventry, United Healthcare, and Time Insurance
entered the market, and the benchmark silver plan increased by 1 percent in the
state. In Michigan, UnitedHealth Care, Physicians Health Plan, and Harbor Health
Plan entered the market, and the average cost of all plans fell by 1
percent.
For silver plans, which accounted for 65
percent of 2014 enrollment nationwide, the average premium was unchanged
from 2014 to 2015. Seven states had double-digit increases in silver plan
average premiums (Alaska, Iowa, Louisiana, Minnesota, New Hampshire, North
Carolina, and Pennsylvania). By contrast, the average silver plan premium
decreased in 17 states (Arizona, Colorado, Connecticut, Georgia, Hawaii,
Illinois, Kentucky, Maryland, Michigan, Mississippi, New Jersey, New Mexico,
Oregon, Rhode Island, South Dakota, Virginia, and Washington).
Average 2015 monthly premiums nationwide are:
- bronze plan—$256
- silver plan—$314
- gold plan—$369
- platinum plan—$441.
The state with the lowest average premiums for silver plans is Hawaii ($206)
while Alaska had the highest average premiums ($583).
Changes in Benchmark Silver Plans
From 2014 to 2015, the nationwide average of premiums for the benchmark plans
was also unchanged (Exhibit 2). While two states, Alaska and Minnesota, had
double-digit increases in the cost of the benchmark plans, many more states saw
decreases. Premiums for the benchmark plan declined in 20 states, with six
states having double-digit decreases (Colorado, Connecticut, Mississippi, New
Hampshire, New Mexico, and Rhode Island).
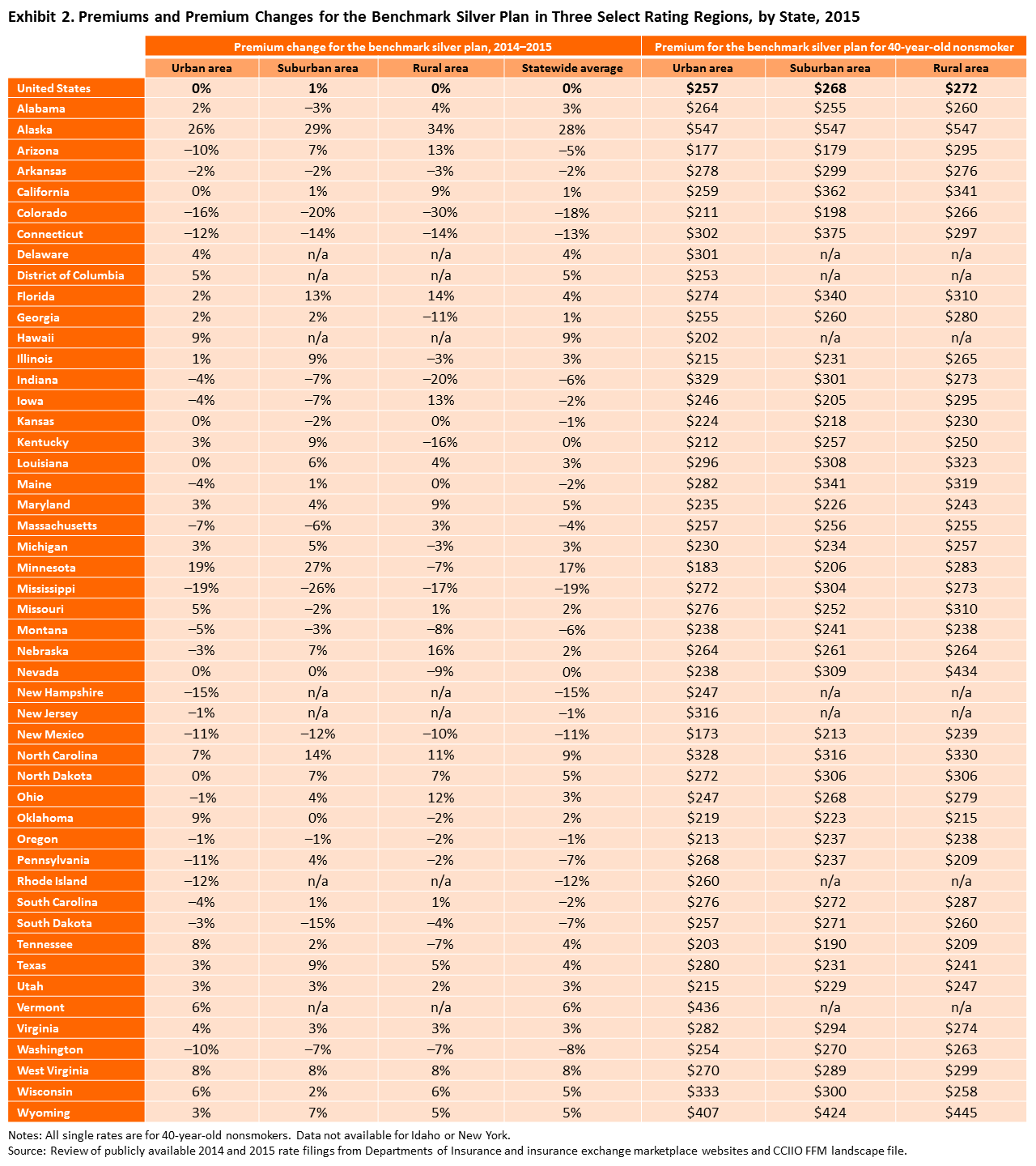
Urban, suburban, and rural rating regions experienced similar premium
changes. Nationally, the average cost of a benchmark silver plan in 2015 is $257
in urban areas, $268 in suburban areas, and $272 in rural areas.
Changes in Deductibles
Nationally, average deductibles increased by 1 percent from 2014 to 2015,
though, again, changes in deductibles varied considerably from state to state
(Exhibit 3). Slightly more states saw increases than decreases (26 states versus
19). Massachusetts and Hawaii had the highest rates of increase in the average
deductibles, at 32 percent and 28 percent, respectively. Washington, D.C.,
residents saw the greatest decrease—with average deductibles down by 16 percent.
In 2015, bronze plans have average deductibles of $5,203; silver plans, $2,965;
gold plans, $1,215; and platinum plans, $552.
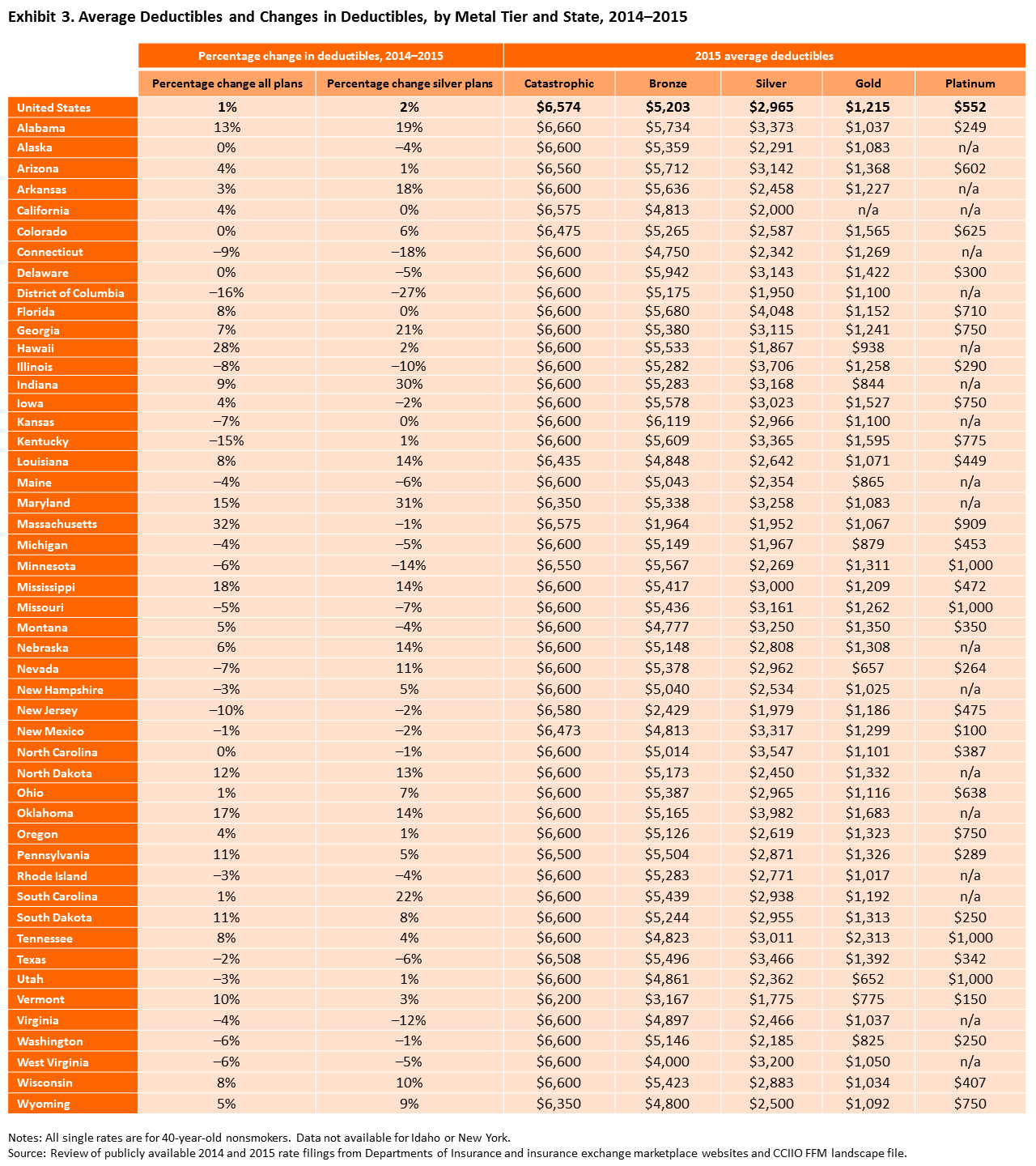
Among silver plans, average deductibles increased in 26 states and declined
in 20 states. The changes ranged from increases of 31 percent and 30 percent
(Maryland and Indiana, respectively) to a decrease of 27 percent (Washington,
D.C.). There is substantial variation among states in average deductibles among
silver plans, ranging from $4,048 in Florida to $1,775 in Vermont. Much of this
variation is because of other aspects of the benefit package, such as copayment
or coinsurance levels.
Carrier Participation
The number of plans offered nationwide increased by 25 percent (not shown).
Fifty more carriers offered plans in urban areas—an average of one additional
carrier per state in 2015 (Exhibit 4). Georgia, Indiana, New Hampshire, and Ohio
saw the largest increase in the number of participating carriers. Increases were
seen across all types of geographical areas. For the selected urban rating
regions, 29 states had increases in the number of participating carriers, while
just three had a decrease, and 17 states experienced no change in the number of
carriers. For the selected suburban areas, 23 states had an increase in the
number of participating carriers, and only four had a decrease. For selected
rural rating regions, 27 had increases and three had decreases.
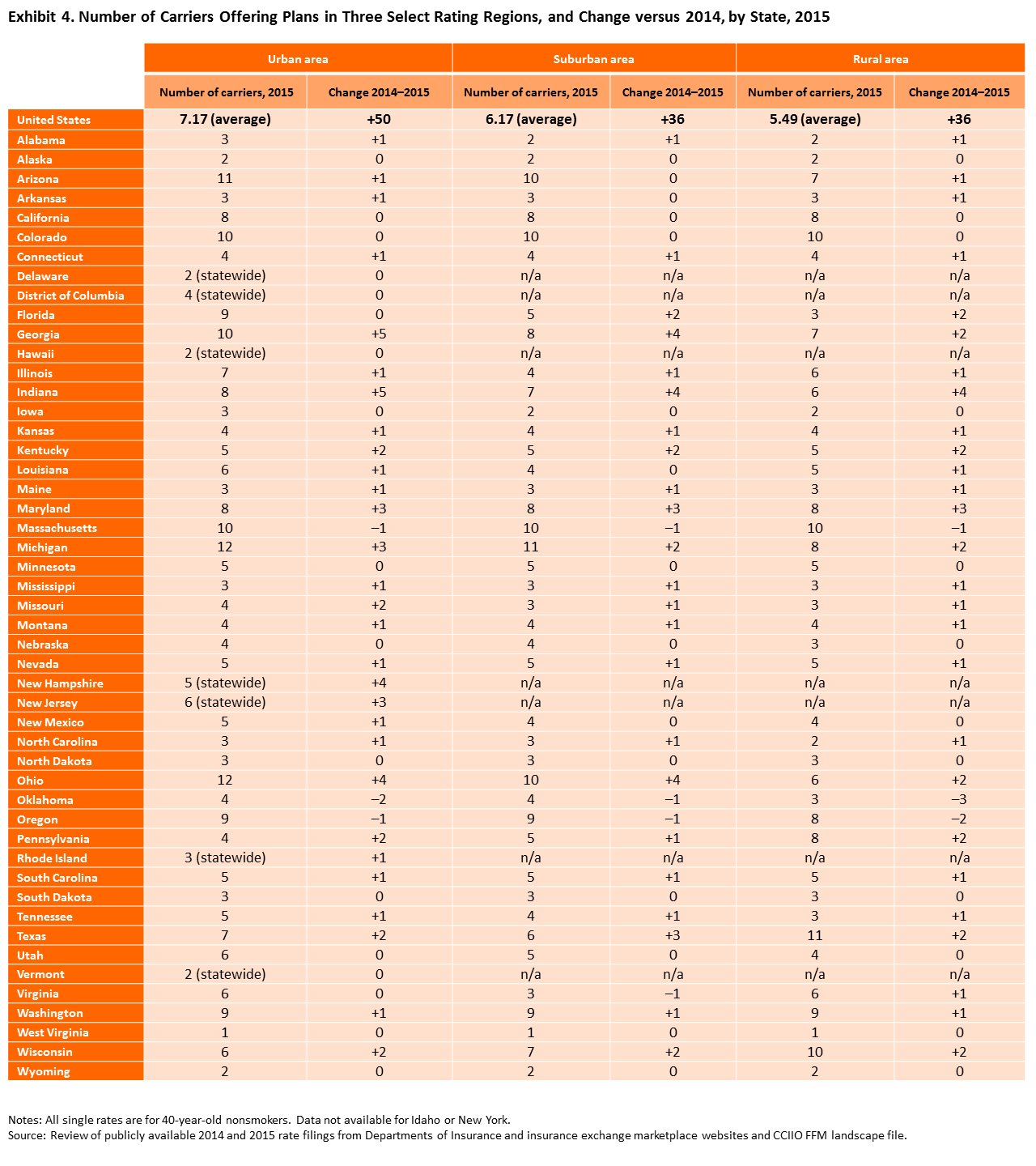
City dwellers have a few more health plan options than their counterparts in
suburban and rural areas. Nationwide, the average number of carriers
participating in urban rating regions is 7.17, versus 6.17 in suburban and 5.49
in rural rating regions.
Behind the Numbers
Why are marketplace insurance costs stable at a national level? One factor is
the way the Affordable Care Act structured the marketplaces. Greater
standardization of benefits through the metal tier structure, premium and
cost-sharing subsidies that are tied to the silver plans, the transparency of
plan information, and robust enrollment in 2014 are collectively increasing the
competitiveness of the market. Sixty-four percent of enrollees in 2014 chose the lowest or
second-lowest cost plan in their tier.
In addition, the risk stabilization programs, which include risk adjustment,
risk corridors, and reinsurance, diminish insurersf risk of financial losses and
allow them to price their plans more aggressively. The temporary risk corridor
program limits both gains and losses of insurers participating in the
marketplace and the temporary reinsurance program provides stop-loss coverage
when claims expenses for an individual exceed a specified amount. The permanent
risk adjustment program transfers funds from insurers with lower-risk patients
to those with higher-risk patients.
The appeal of the marketplace structure and risk stabilization programs have,
in turn, led to the increase in insurer participation, which also helps to
contain costs.
An outstanding question, however, is the long-term sustainability of current
trends in premiums. Similar to employer-based insurance, long-run developments
in marketplace premiums will follow trends in medical claims expenses per
capita. With the exception of the mid-1990s, the era of restrictive managed
care, claims expenses have historically increased at 5 percent or more per year
(see Appendix). Future price increases of marketplace plans will depend on how
effectively America reforms the delivery of care and moves from a system that
rewards high volume to one that rewards high-quality care.
See the appendix for the study methodology.